The Department of Anesthesiology has experienced great change, monumental success, and many challenges since it was started by Dr. Ralph Waters in 1927. However, the department had not previously endured, responded to, or emerged from a Pandemic. COVID-19 brought challenge and disappointment, and some opportunity, and permanently changed much of what was previously normative in American Anesthesiology. Our memories of this time shape how we will experience the future. This article will examine the impact of COVID-19 on the department and our lives, reflect on some of our memories, and recall the important work we accomplished together beginning in March 2020.
Leadership
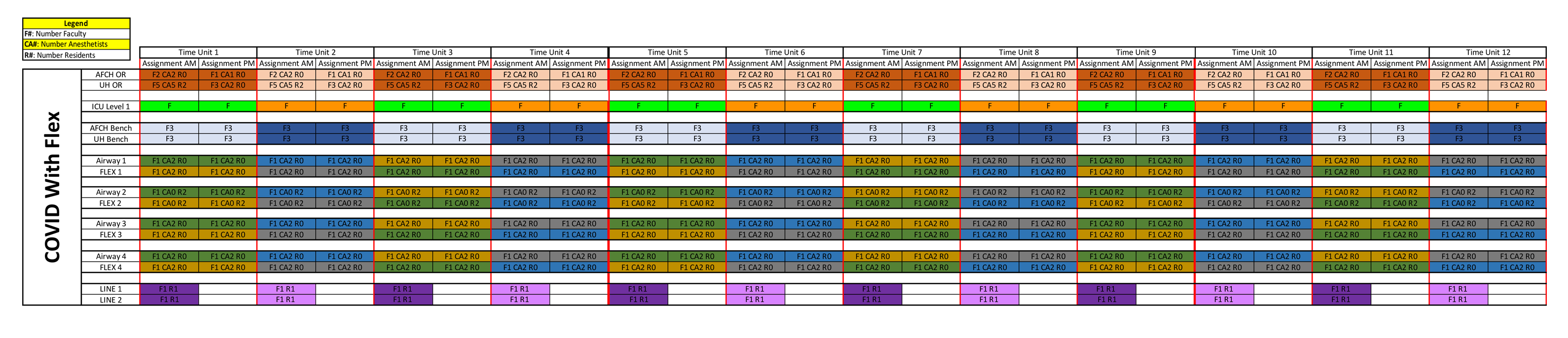
In an interview with Department Chair, Dr. Kelly McQueen, she shared her reflections as a new chair, who was asked to shift the priorities of the department and plan for collaborative operations to meet the needs of the COVID patients who were expected to arrive for treatment. She recalled, “The Chairs of the Departments of Anesthesiology, Emergency Medicine, Medicine, and Surgery worked collaboratively to plan for expanded critical care that was expected to overtake all clinical operations for an anticipated surge of critically ill COVID patients. We participated in a 24/7 coverage model that expanded to include airway and central line strike teams, potentially provide for ICU coverage, and also provide for ongoing urgent and emergency surgery.” See figure 1. She observed that in spite of personal fears and many unknowns, the entire department rose to the occasion and worked within a new schedule of constantly changing demands.
The departmental leadership took on new commitments and roles – writing and re-writing new coverage schedules, providing PPE-appropriate training, and committing to communicating the changing information whenever needed. She explained, “We provided lengthy emails with many, sometimes daily updates. We held virtual updates weekly. And while communication was essential, we constantly felt behind and inadequate to meet the many needs of our residents, our staff, the anesthetists and faculty, and, of course, their families and loved ones.” She noted that “fortunately for our teams and the patients of Madison, the anticipated surge never fully arrived, but the department nevertheless suffered many losses and a degree of burnout and diminished morale not previously experienced.”
PPE and PAPRs

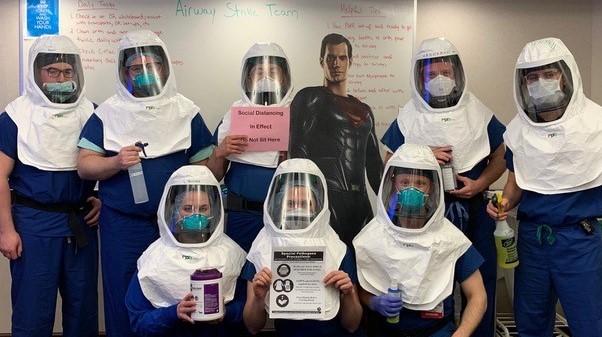
Dr. Lianne Stephenson led the task of organizing the department’s response to limited supplies and the development of Airway Response teams. When asked to reflect on how
she facilitated the collaboration and organization of PPE, PAPRs, disposable Airway equipment, and OR modifications, she began with a reflection on the atmosphere in March 2020. “I remember the contrast of the quiet neighborhoods and streets around the hospital compared to the chaos and uncertainty that existed within the hospital,” she said and went on, “It felt like everything was moving so slowly, but in retrospect, both the hospital and department made changes really quickly.” She expressed, “I will never forget all the staff who helped make and implement all of the new protocols.”
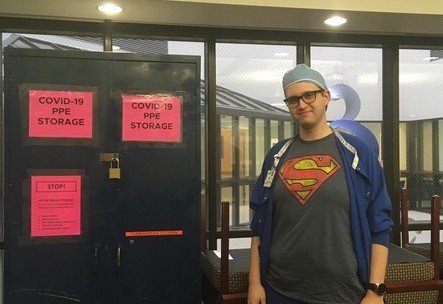
She described how the Orth conference room was transformed into ‘PPE central’ by UW-Health’s Jayson Greenwood, Clinical Engineer Anesthesiology. “Jayson’s support in identifying a reliable alternate source of PAPRs and hoods kept our department members safe from infection and was mission-critical,” she said thankfully. Additionally, she remembered other specific contributions, including that of Austin Gokey, an Anesthesia Technician. She described, “In a matter of weeks, he successfully performed an enormous outreach effort to provide documentation and to train all clinical department members in the safe use of PAPRs.” She noted that during COVID, “Nothing stayed the same, and eventually, we learned to adapt. It was definitely challenging in the beginning.”
Perioperative Services

Dr. Christopher Tuner, UW Health Director of Perioperative Services-Anesthesia, shared his experiences of March 2020 through a podcast interview, “First Case, the Operative Room Podcast” from the Fall of 2020. He felt it captured his perspective during this time accurately. He began the interview as he described the time in detail “at the onset of Covid-19 last spring, the OR triad system (consisting of the OR charge nurse, an anesthesiologist, and a surgeon) quickly identified that we needed a coordinated response in
managing both surgical and procedural volumes based upon the conditions on the ground.” He explained that the University Hospital OR triad was asked to create and lead the surgical and procedural services workgroup tasked to monitor surgical and procedural activity across the system. He revealed in the interview that this included cutting back considerably on operating room staff and repositioning anesthesia physicians and staff to critical care and critical care strike teams.
He recalls in the interview candidly, “When COVID started, my analogy for this place is the “Battleship Wisconsin,” which is very big and very impressive and very good at steaming straight but doesn’t turn all that well.” He declared in the interview, “I had to eat my words… because we essentially, over the course of 3 or 4 weeks, completely reconfigured this hospital from a standard academic quaternary medical center into a COVID critical care hospital.”
Scheduling and ICU Coverage

When asked to reflect on the Spring of 2020, Department Vice Chair of Clinical Affairs, Dr. Martha Wynn, describes in detail how scheduling was impacted. She noted, “during the first phase of the COVID pandemic, the Department of Anesthesiology was asked to schedule faculty, residents, and CAs on a 5-days on, 10-15 days off Block schedule at each inpatient hospital in order to provide 24-hour OR coverage for urgent and emergent surgeries and allow recovery time between Blocks worked.” She revealed that the COVID block schedule, as shown in figure 1, provided flexible ICU coverage when needed. She reflected, “The COVID Block schedule was demanding and stressful, but the anesthesiology teams proved to be resilient and committed.”
Additionally, she noted, “during COVID, the Department also scheduled an airway response team at each hospital.” As a result, she mentioned that the airway team has become an established and valued patient care team at University Hospital.
Education and Training

The profound effect COVID had on the education and training of residents during the Spring of 2020 was captured by an account from Dr. Christopher Darling, Residency Program Director. He recalled working with department leadership to identify available trainee efforts that could be redeployed. According to Dr. Darling, “one way to continue
learning virtually during this time was by using WebEx.” He recalled the plethora of changes during this time and explained, “with guidance for our Department Vice Chair of Clinical Affairs, Dr. Martha Wynn, we were constantly updating the schedules.” He remarked, “I probably rewrote them 10 plus times which was one of the most time-consuming tasks I was responsible for.” He reflected broadly upon the Spring of 2020 and noted, “In general, everything changed. We adapted to daily and weekly check-ins with the residents to update them on any developments in the department”.
“On a personal level,” he explained, “life during a pandemic brought on unforeseen challenges.” For example, he expressed, “I had specifically asked to work nights so I could be available during the day because I had no childcare.” He added jokingly that “an unexpected result of his new ‘night shift’ was troubleshooting residency issues and finding times when other people were actually awake.”
Administrative and Fiscal Operations
Will Katz, Department Administrator, was asked to reflect on March 2020 and walk us through the impact it had on the administrative and fiscal operations of the Department.
He first described the administrative staff impact, and he recalled, “with literally a day or two of notice, our administrative staff transitioned to a remote workforce.” He explained that change and uncertainty were the only constants for several months. He noted, “daily, we would respond to multiple updates and changes in guidance and direction from SMPH, UW Health, and the CDC.” “The main focus was balancing effective support of our clinical providers who remained on-site, with the health and well-being of our administrative team,” he said. He noted the significant challenge of operationalizing a new normal and rapidly assimilating secure remote access, virtual platforms, and infrastructure. He reflected further, “It is hard to imagine now, but the reality is that WebEx, Zoom, Teams, the use of webcams, etc. were very new to all of us at that time”. He continues, “In short, it was one of the most unsettling times we have endured. A huge kudos to all of our administrative staff and leaders who made the transition as seamless as possible!”

Next, he recounted the effects of fiscal operations during this time. He recalled, “consistent with the harsh global economic impact, UW health and SMPH faced unprecedented fiscal realities which resulted in numerous, fast-paced changes at every level of the department.” He illustrated, “for example, clinical faculty, anesthetists, and NPs faced a mandated reduction in compensation in May and June 2020, and all SMHP employees endured two rounds of mandated furlough days spanning from May 2020- June 2021. UW Health staff were mandated to reduce their hours worked, and the department faced a mandated 10% reduction in other operating expenses in FY21.” He expounded upon how the reduced operating budget manifested in lesser CME allowances for clinical providers, a reduction in professional development for administrative staff, a travel ban, and canceled holiday parties, summer picnics, and other social gatherings.
“Despite the monumental challenges,” he revealed, “I am proud of the cross-functional collaboration and tireless effort of all who helped ensure effective administrative and responsible fiscal operations.” He further recalled, “Of the many challenges, I vividly remember the collective long hours and late-night efforts of many to align ‘the COVID block schedule’ with the respective compensation structures to ensure the minimal overall impact to clinical faculty and clinical anesthetist compensation.” In final reflection, he concluded, “Certainly, our efforts were not all perfect; however, I am grateful for what we learned, and remain in awe of, and have great respect for all that we accomplished. I feel we are better for having gone through this together.”
Vaccine Clinical Trials and Community Outreach
Dr. William Hartman was asked to reflect on the Spring of 2020. He described the time from his unique perspective, which included contributions to the pandemic, including
clinical trial involvement and subsequent outreach to the local community. This local opportunity quickly morphed from a local spokesperson for ‘all things COVID role’ in the Spring of 2020 to a national and international expert on COVID treatments and vaccines as the pandemic persisted.
He explained his clinical trial journey in 3 phases during the entirety of the pandemic. The first phase was being a part of a national convalescent plasma program. He noted, “we were the third or fourth hospital in the country to use CCP.” The next phase included investigating monoclonal antibodies for inpatients, outpatients, and for prophylaxis. He revealed, “we were one of the first hospitals to do this.” The last phase was the vaccine for COVID-19. He added, “I ran the adult and pediatric COVID vaccine trials- the only COVID trials in Wisconsin.”
Well-Being

The department had a wellness committee prior to the beginning of COVID-19, and we had excellent champions in Dr.’s Head, Popic, and Warren. Proximal to the beginning of COVID-19, a departmental traumatic event, gave us the opportunity to appreciate the role of a Peer-Support Network, and we quickly committed to training interested department members to become Peer Supporters. The Pandemic gave us the opportunity to have a renewed commitment to well-being. The Wellness Committee members rallied for opportunities to support well-being; food was centric to this effort, while other creative endeavors, such as the plant distribution from Will Filbey, offered the hope found in living things. In spite of our best intentions and commitment, however, there is no doubt that the wellbeing and morale of the department have suffered. We know that our profession has suffered across the US and Globally secondary to our role in responding to the Pandemic. With this knowledge, we will remain committed to supporting each other and ourselves as we continue to recover. Burnout and decreased morale, and even loss of purpose, are realities in our department and profession, and acknowledging these realities are essential to a future that reduces burnout and improves morale. Annually we will explore opportunities that support our commitment to well-being.
In Final Reflection

In this collection of photos and experiences, Dr. McQueen emphasized, “I hope we have captured some of the highs and lows of our Department during the most active phase of COVID-19.” She further reflected on the time period, “Our commitment to a common goal was representative of our professionalism and resilience, but it took a toll on individuals, teams, and families, and this is an important part of our COVID story. We lost team members acutely to retirement and to care for family members; we suffered from fear and burnout, and for many, if not most, our lives were permanently altered.”
There were many heroes within the Department of Anesthesiology, and all of their stories deserve to be memorialized. Our sincere hope is that this article will contribute to archiving this chapter of our historical department. Collectively we can take pride in the dedication and personal sacrifice witnessed during the days and nights of the Pandemic.