The world needs a better way of identifying which patients will benefit from a blood transfusion. For over 100 years, doctors have transfused red blood cells to improve tissue oxygenation without knowing reliably whether a patient’s oxygenation was poor. Choosing to transfuse based on the blood hemoglobin level – the sole and traditional method – results in over 33% of transfusions being misdirected, wasted, and even harmful. Using tissue oxygen consumption to guide transfusion improves the safety and efficacy of blood, but no one has yet achieved a practical noninvasive technique. Our lab studies new ways to measure oxygenation at the bedside. In collaboration with the Department of Mechanical Engineering at the University of Canterbury, we are developing a prototype noninvasive oximeter that can accurately measure both peripheral and cerebral oxygen extraction.

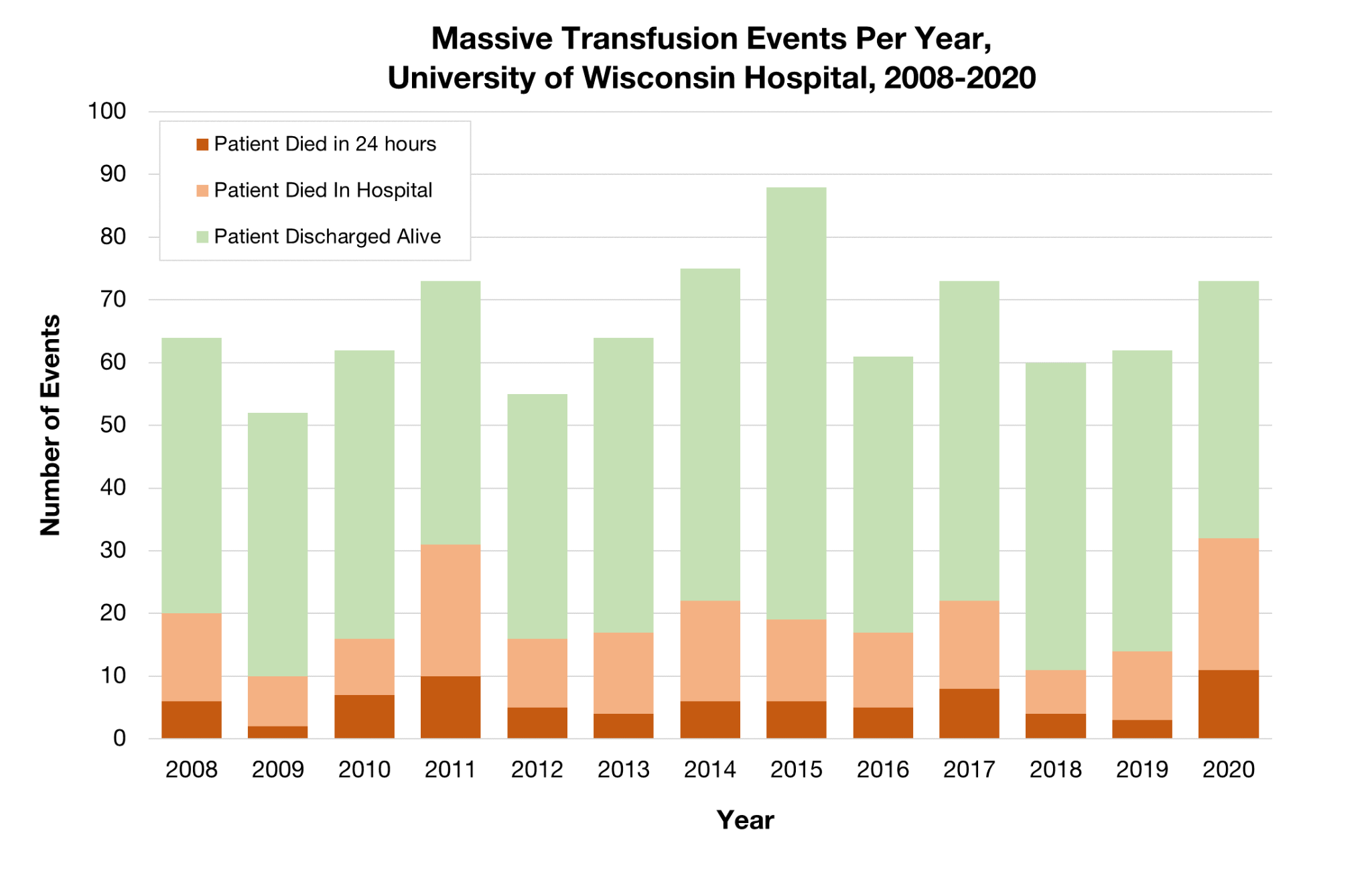
We also research risk factors, methods, and outcomes in massive resuscitation. Although most people imagine a young trauma patient, most massive resuscitations are given to older patients having major surgery or medical procedures. In collaboration with the Multicenter Perioperative Outcomes Group, we are leading the largest-ever observational study of transfusions in American surgical patients, looking at blood use, massive transfusions, and outcomes.
Dr. Hess’ lab has also joined in collaborative work on platelet mitochondrial genetics, patient “health numeracy”, and the uses of large language models in making accurate clinical decisions about transfusion medicine.
More Info
![]()
Aaron Hess, MD, PhD
Assistant Professor
Department of Anesthesiology
University of Wisconsin
(608) 265-7002